- 1300 478 375
Menu
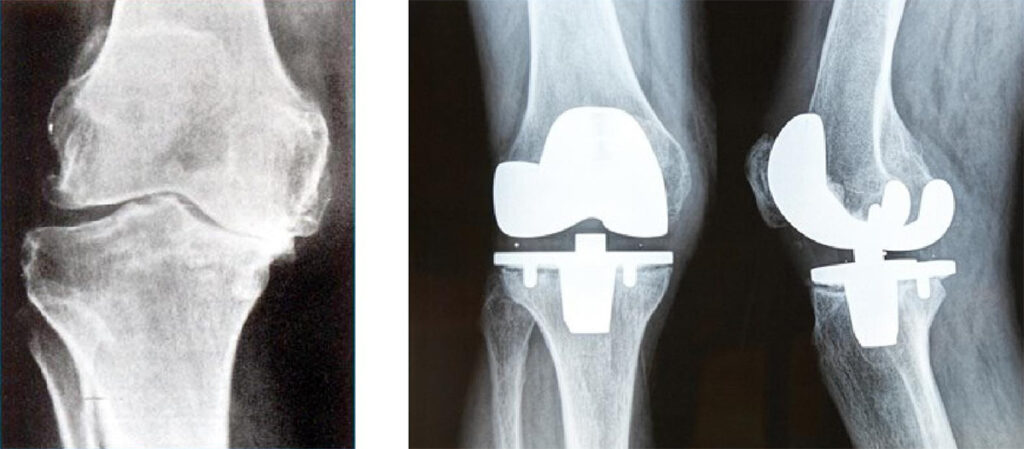
The reason for having a total knee replacement is to replace a painful and badly worn (arthritic) knee with an artificial joint that will allow pain free walking and activities of daily life. If performed well and appropriately cared for following the surgery, your knee replacement should provide you with many years of quality life and relief from pain.
It is important to realize that an artificial knee will never function in exactly the same manner as your original and your doctor’s advice regarding care for your artificial knee should be followed. The artificial knee is made of metal (chrome cobalt or titanium) and a plastic (high density polyethylene) joint bearing that will slowly wear over the years. If too much wear occurs the knee may become loose and painful or the components may even break. Often in the early stages there are no symptoms of wear or loosening and these may not present until irreversible damage is done. It is important to treat your knee carefully and avoid excessive activities that may shorten the life of your artificial joint. Activities such as running, tennis, aerobics or other high impact activities should be avoided. Walking for exercise, the use of an exercise bicycle and swimming are excellent for your overall general health and not detrimental to your artificial knee.
Please ensure that you have read the above information carefully and discuss any questions arising from this with your doctor prior to embarking upon your operation.
This is a guide to your upcoming operation. In it we explain what is likely to happen at each stage of the process. However your care will depend on your individual needs, so your progress may vary from this basic outline. Please become familiar with this guide and discuss any aspects you wish to with your surgeon or the nursing staff.
You will be admitted on the morning of surgery, unless this is impractical or you have some significant medical problems. You should expect to be in hospital for three to five days, depending on the speed of your rehabilitation.
You should stop taking anti-inflammatory drugs at least five days prior to surgery as they can increase the risk of bleeding. These tablets include Voltaren, Nurofen, Brufen, Feldene, and Indocid (Celebrex is not a problem). If you are on low-dose aspirin (eg. to prevent stroke or heart attack) you may continue to take these.
You should keep the skin near the operation site clean. If you have a cut or pimple on the skin in the area, you should notify your surgeon prior to surgery.
You should not eat or drink 6 hours prior to surgery admission. (You may not be the first patient on the list, but the order may need to be changed unexpectedly)
You should bring with you
If you wish, your surgeon will speak to a family member in person or on the phone after surgery. Please notify the nursing staff of the details.
When you return to the ward, you will be resting in bed. You will have a drip in your arm for fluids. You will have a bulky dressing over the wound on your knee and special stockings on your legs designed to help reduce the risk of blood clots forming.
On the day following surgery you will have a check blood count and an x-ray of the appropriate knee performed. Under the guide of the physiotherapist you will be stood up and usually take a few steps. Sometimes patients may have a strong reaction to the anaesthetic which may result in continuing nausea and thus delay your first steps for another 24 hours.
You will be commenced on a single aspirin tablet a day (300mg) to be taken with food. This will be continued for six weeks and is designed to help thin the blood slightly and prevent blood clots in the legs or elsewhere.
When the results of the check blood count are back, sometimes extra blood is required. This will be given into a drip that remains in your arm from the time of surgery.
The physiotherapist will take you for a walk and give you instructions about your activities during the recovery period, including an exercise programme. For pain control you will have injections (Morphine) and tablets (Panadeine Forte) available. Most people require either no injections or only one or two, as tablets are usually enough to control the pain.
By day three to five most patients are ready to go home. By this stage patients can safely get into and out of beds and chairs and go up and down stairs. Some patients may require changes to their housing, such as ramps or rails or aids in the bathroom. This should be discussed with your doctor prior to the surgery so that appropriate arrangements can be made and that delays will not interfere with your departure from hospital. For patients going home on their own, interim help can be arranged with home provision of meals and help bathing if required. Again, please let your doctor know well in advance if you feel that this form of help may be of assistance for you. Many patients are fortunate enough to have family living close by who are able to help with meals and accommodation for a few weeks while your strength and mobility return. This can make the transition from the hospital to home less difficult and again thought should be given to this well prior to the time of surgery.
You can expect some pain at the site of the operation. It usually gradually decreases in the first few weeks and is not as severe as the pain was before surgery. This is normal and you should not be concerned. You may take the tablets given to you as needed for pain.
You should take the dressings off after 12 days following surgery. If it falls off before this and the wound is clean, you should not worry. There are usually no stitches to remove as they are dissolving and under the skin. As the body dissolves the stitches, there is sometimes a mild reaction around the wound, seen as some redness and inflammation. The wound should be kept clean and dry until the wound is completely healed (12 days): an appropriate waterproof covering should be employed while in showering and submersion of the wound in a bath or pool should be avoided.
If at any time the wound becomes hot, red or swollen or begins to ooze fluid Dr Sterling (or local doctor) should be immediately contacted.
You should wear your stockings for six week.
You should follow the guidelines given to you by your physiotherapist with regard to physical activity and exercise. For the first four weeks, you should spend most of the time resting at home, alternating between lying down and sitting. After this, you should increase your activity level slowly with an aim to be back to most activities at six weeks. You should be safe to drive at six weeks following your first post- operative review by your orthopaedic surgeon. You will be reviewed by Dr Sterling six weeks after surgery.
You should contact Dr Sterling if:
Following your return home you should contact the Rooms (1300 478 375) and make an appointment for your first post-operative review at six weeks following your surgery. You are able to be driven in the family car for this trip (if there are any concerns regarding this please ring first.
Your new knee then requires regular “check-ups”, something akin to the regular services that you have performed on your car. You should be seen next at 6 months and then every year thereafter following your operation. At each of these visits your should have x-rays of your knee performed beforehand to take along. Your local doctor is able to arrange for these x-rays to be performed. Again if you have any concerns please do not hesitate to ring and a form can be mailed to you prior to your visit.
The exercises are designed to help you regain full range of movement and muscle strength in your leg. It is equally important to be able to bend your leg fully as it is to get it fully straight, and particularly to be able to lock the knee straight.
Build up the repetitions of each exercise gradually and aim for two 10 minute sessions per day.
Static Quads Exercise: Sit on the bed/floor with your leg straight out in front. Use your thigh muscles to press the back of your knee into the bed/floor as hard as you can. Keep your toes pulled up towards your body. Hold for 5 seconds relax completely and repeat.
You may have moderate pain following the surgery and can take panadeine forte as provided or paracetamol.
The pain should lessen each day. You should contact Dr Sterling (through the switchboard of the hospital where you had your surgery), or his secretary on 1300 478 375.
Whilst it is unlikely, if you feel extremely unwell, or there is an unexpected delay in finding Dr Sterling, attend the nearest Hospital Emergency Department.




Take the first step towards your treatment and book your initial appointment with our orthopaedic surgery team.
Prefer the phone? 1300 478 375


